Hysteroscopy
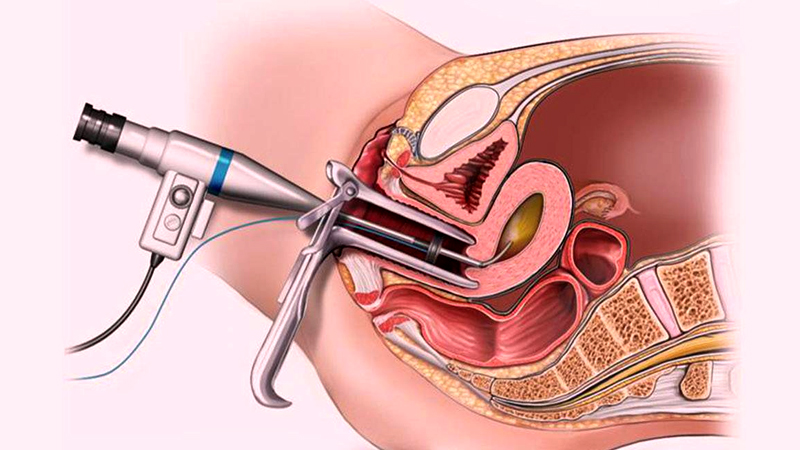
Hysteroscopy is a minimally invasive procedure used to examine and treat problems inside the uterus. It involves the use of a hysteroscope, a thin, lighted tube that is inserted through the vagina and cervix into the uterine cavity. Hysteroscopy can be either diagnostic or operative, depending on the purpose of the procedure.
Indications
Hysteroscopy is indicated for:
- Abnormal Uterine Bleeding: To investigate causes of heavy, irregular, or postmenopausal bleeding.
- Fibroids or Polyps: To diagnose and remove benign growths in the uterine lining.
- Uterine Anomalies: To examine and correct congenital abnormalities, such as septate uterus.
- Infertility Evaluation: To investigate potential causes of infertility or recurrent miscarriages.
- Retained Products of Conception: To remove remaining tissue after a miscarriage or delivery.
- Endometrial Ablation: To treat heavy menstrual bleeding by destroying the uterine lining.
Procedure
Diagnostic Hysteroscopy
- Preparation: The patient may be given a sedative or local, regional, or general anesthesia.
- Insertion: A speculum is inserted into the vagina to visualize the cervix. The hysteroscope is then gently inserted through the cervix into the uterine cavity.
- Inspection: The uterine cavity is distended with a saline solution to allow for clear visualization. The hysteroscope transmits images to a monitor, enabling the doctor to inspect the uterus for abnormalities.
- Completion: The procedure usually takes 10-30 minutes and is often performed on an outpatient basis.
Operative Hysteroscopy
- Preparation: The patient is given anesthesia, usually general or regional.
- Insertion: Similar to diagnostic hysteroscopy, a hysteroscope is inserted into the uterine cavity.
- Treatment: Special instruments are passed through the hysteroscope to perform necessary treatments, such as removing polyps or fibroids, cutting adhesions, or correcting uterine anomalies.
- Completion: The procedure may take longer than diagnostic hysteroscopy and may require a short recovery period in the hospital.
Recovery
- Postoperative Care: Patients are monitored for a short time after the procedure until the effects of anesthesia wear off.
- Activity: Most patients can resume normal activities within a day or two, though heavy lifting and strenuous activities should be avoided for a few days.
- Follow-up: A follow-up appointment is typically scheduled to discuss the findings and any further treatment needed.
Benefits
- Minimally Invasive: Small instruments and no abdominal incisions result in less pain and quicker recovery.
- Accurate Diagnosis: Provides direct visualization of the uterine cavity for accurate diagnosis.
- Simultaneous Treatment: Allows for both diagnosis and treatment in the same procedure.
Risks and Complications
- Bleeding: Mild bleeding or spotting may occur after the procedure.
- Infection: There is a small risk of infection.
- Uterine Perforation: Rarely, the hysteroscope or instruments can create a hole in the uterus, which may require further surgery.
- Fluid Overload: During the procedure, the fluid used to distend the uterus can be absorbed into the bloodstream, causing fluid overload.
Alternatives
- Ultrasound: Transvaginal or pelvic ultrasound can provide images of the uterus and detect abnormalities.
- Sonohysterography: A saline infusion ultrasound that provides clearer images of the uterine cavity.
- MRI: Magnetic resonance imaging can offer detailed images of the uterus and surrounding structures.
- Dilation and Curettage (D&C): A procedure where the cervix is dilated and tissue is scraped from the uterine lining, used for diagnosis and treatment of uterine conditions.
Patients should discuss their symptoms, medical history, and the potential benefits and risks of hysteroscopy with their healthcare provider to determine if it is the appropriate diagnostic or treatment option.
